Stethoscope and Adhesive Note With Text Medicaid. (Via Getty Images)
A nor’easter of Medicaid cuts is poised to slam into Seacoast area nursing homes on Jan. 1.
It had seemed nursing home care was spared the carnage afflicting many other areas of the two-year state budget that took effect on July 1. Despite tight revenue, New Hampshire Gov. Kelly Ayotte and state senators made it a point of rejecting House-passed Medicaid cuts. And the appropriation for nursing home care represented a modest increase from the prior state fiscal year, resulting in a heartening 2.4% increase when the budget took effect.
However, as it turns out, that increase was illusory, because now it will be more than clawed back by a funding shortfall. While the average Medicaid cut would be 3% on Jan. 1, that figure really does not tell an accurate story. Many facilities would experience much more severe cuts that are sure to result in closures.
Whether for-profit or nonprofit, Seacoast facilities would get blasted, including the county homes. The Rockingham County Rehabilitation & Nursing Center would see a 11.72% cut, or a loss of $34.02 per resident, per day. Strafford County’s Riverside Rest Home would be cut by 6.47%, or $16.50 per resident, per day.
In Dover, the nonprofit St. Ann Rehabilitation and Nursing Center would, like other facilities run statewide by Catholic Charities New Hampshire, take an enormous hit – a 12.74% cut robbing care resources by $34.43 per resident, per day. The nonprofit Webster at Rye would suffer the area’s worst blow, a 16.18% cut, or $47.22 per resident, per day.
State cuts of this scale are completely untenable, and utterly inconsistent with what legislators’ expectations were. Money must be found to stop them. Daily cuts of the magnitude I describe very quickly would become new annual losses soaring to several hundred thousand dollars per facility. That would be on top of the money-losing proposition that caring for the state’s most vulnerable Medicaid beneficiaries already is.
Nursing homes have incurred huge costs since the COVID-19 pandemic began, and Medicaid reimbursement has not kept pace despite good-faith legislative efforts to improve it. In the past five years, hourly wages have gone up an average of over 35 percent, and yet facilities still have not recovered their pre-pandemic workforce.
Just over half of all nursing home workers are licensed nursing assistants, but even with wages no less than, say, around $23 an hour it can be awfully hard to find a LNA. State budget limitations have curbed health care workforce development. On the Seacoast you have the added challenge of housing unaffordability and unavailability discouraging prospective caregivers.
Other costs have soared too. For example, we’re all familiar with the fact that eggs are more expensive – with the most recent federal data showing that a dozen cost 238% more than they did five years ago. So, imagine making breakfast for over one hundred people each day. There are innumerable other costs associated with caring for, and feeding, residents that have soared.
In this state with the nation’s second-oldest population, facilities work overtime to be efficient within provided Medicaid means – but the strain can be unbearable. Do we really want the first care cuts since January 2015, and the first nursing home closures since 2016? Given our aging population, this is not the time to go backwards. Our policymakers must intervene and spare the frailest Granite Staters from disaster.
Brendan Williams is the president and chief executive officer of the New Hampshire Health Care Association.
This article originally appeared on Portsmouth Herald. Reporting by Brendan Williams.
GOP midterm candidates turn on affordable health care
Republicans running for 2026 would raise out-of-pocket premiums and weaken consumer protections while others want ACA scrapped. A number of...

OPINION: All Granite Staters Deserve Real Access to Preventive Health Care
As Breast Cancer Awareness Month comes to a close, we are reminded that awareness alone is not enough – especially for Black women, who experience...

With health care tax credits set to expire, pain sets in for one New Hampshire business
By William Skipworth / New Hampshire Bulletin Last week, W.H. Bagshaw, a metal parts manufacturer based in Hudson, found out that its health...

A new car vs. health insurance? Average family job-based coverage hits $27K
By Phil Galewitz, KFF Health News With the federal shutdown entering its fourth week, spurred by a stalemate over the cost of health insurance for...

NH Dems blast ‘reckless’ GOP shutdown, warn of rising health costs for Granite Staters
Speakers warned that a dual-income couple could face a nearly $15,000 increase in costs if Affordable Care Act tax credits expire. Democratic...
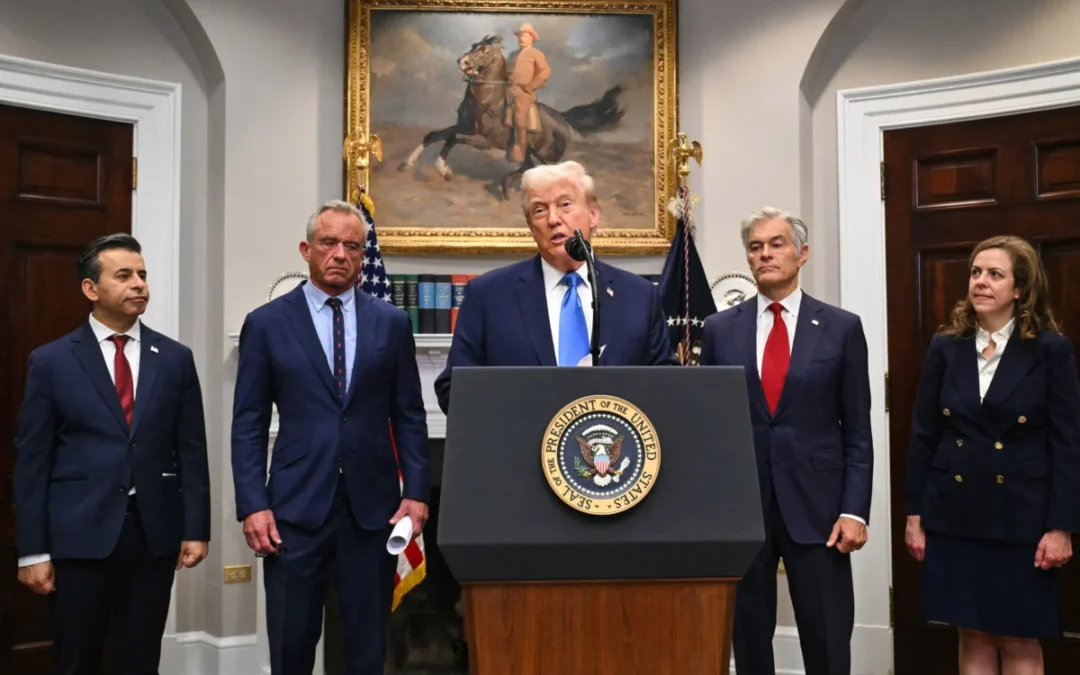
We asked, you answered: What do you think about the president’s claims that taking Tylenol while pregnant causes autism?
A version of this story appeared in the Granite Post's newsletter. Subscribe here. President Donald Trump announced Monday, Sept. 22 that the Food...