
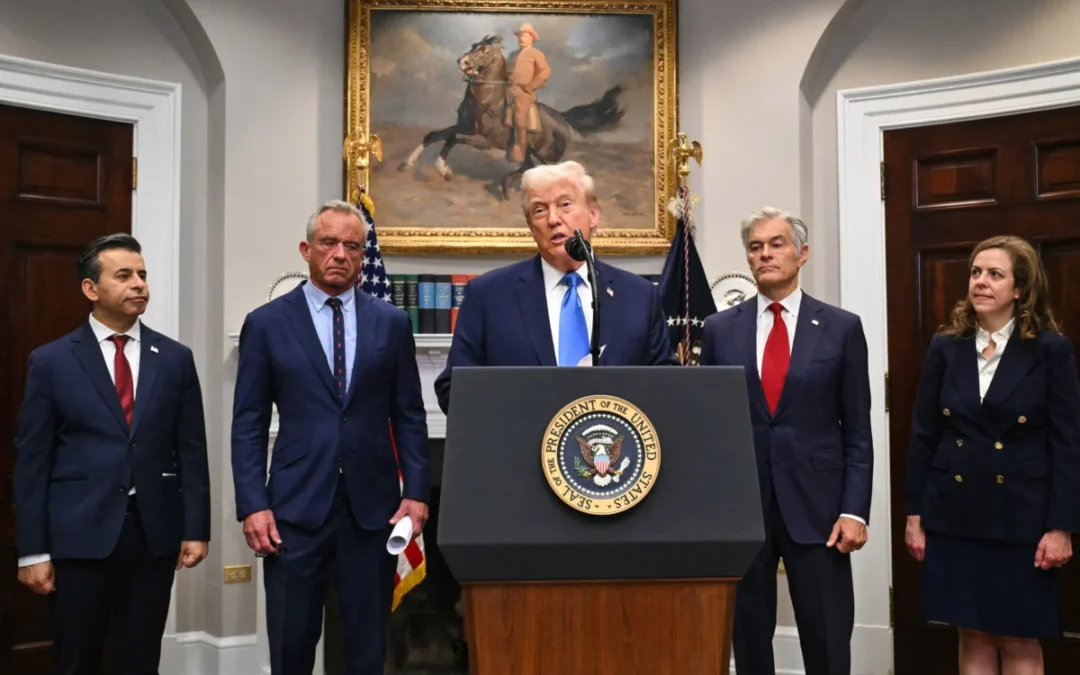
A vial of coronavirus vaccine on a vaccination record card with a syringe on the side
Nathaniel Weixel of The Hill reported that the federal government was ending its program to offer free COVID vaccinations to underinsured and uninsured individuals. The program was meant to end in December 2024; however, it is set to end in August. Those who wish to have a COVID vaccine this year and cannot afford out of pocket costs will have to do so before September 2024.
In 2023, after the federal government provided all the costs of producing vaccines for companies like Moderna and Pfizer, those companies decided to start charging around $130 for each vaccination. Previously, they had cost around $32. The vaccinations have quadrupled in price.
While Moderna announced it would begin offering vaccinations for free to those who could not afford them beginning in May 2023, accessing those free vaccines would most likely require a caseworker or assistance of some description for a person to take advantage of the offer. Senior citizens and homeless individuals are among those less likely to have access to a computer and willingness to discover new information for themselves. They would have had to have been told directly by someone about the offer.
Vaccination refusal and/or disbelief has become increasingly prevalent in America, as senior citizens refuse to get a COVID vaccine, despite being most at risk of dying from it. Additionally, those who wish to continue with yearly vaccinations may find it difficult to do so if they do not have health insurance- a number which constituted roughly 25 million Americans as of 2023.
Unlike other vaccines, a COVID vaccination will not prevent a person from getting the disease; rather, the disease will be far less deleterious in the presence of antibodies already present.
For those who get sick and did not have a vaccine, a Pfizer drug called Paxlovid received FDA approval to help treat those at risk for hospitalization and death due to COVID. Those most at risk are senior citizens who refused a vaccine and may not have sufficient funds to pay out of pocket costs.
In October 2023, Pfizer started charging $1,390 for Paxlovid. The company did offer an assistance program for those who could not afford the drug; however, after a COVID infection in May 2024, I found the price at a local Rite-Aid pharmacy had risen to $1,600. What was more, New Hampshire’s AmeriHealth Medicaid program would not cover the cost of the prescription.
To gain access to the drug, I would have to register online for Pfizer’s co-pay savings program, fundraise, or find some other way- if I did not already happen to have around $2,000 just lying around waiting to be spent.
Since I am not a senior citizen or at-risk individual, perhaps I will be okay without the medicine. Perhaps having several vaccines over the years will protect my health. I may come out the other side of contracting COVID like many others had: a long bout of a strong cold or flu during a time of self-isolation followed by a return to normalcy.
If I were an at-risk person without a vaccination, circumstances might be different. I might find myself receiving a message from a friend who went to the pharmacy saying the drug a doctor told me I needed to stay alive was too expensive and not covered by my insurance plan. I might be forced to tough it out, even if that meant a drop in oxygen levels followed by shortness of breath and coughing up blood.
I might have to be admitted to a hospital for an intubation procedure- the opening of a hole in a person’s neck so a breathing tube can be placed in it- just so that I could breathe. I might die for entirely preventable reasons- partly my own fault for not accessing vaccinations when I could have, and partly due to the price of Paxlovid rising well beyond what an average person could afford out of pocket.
We asked, you answered: What do you think about the president’s claims that taking Tylenol while pregnant causes autism?
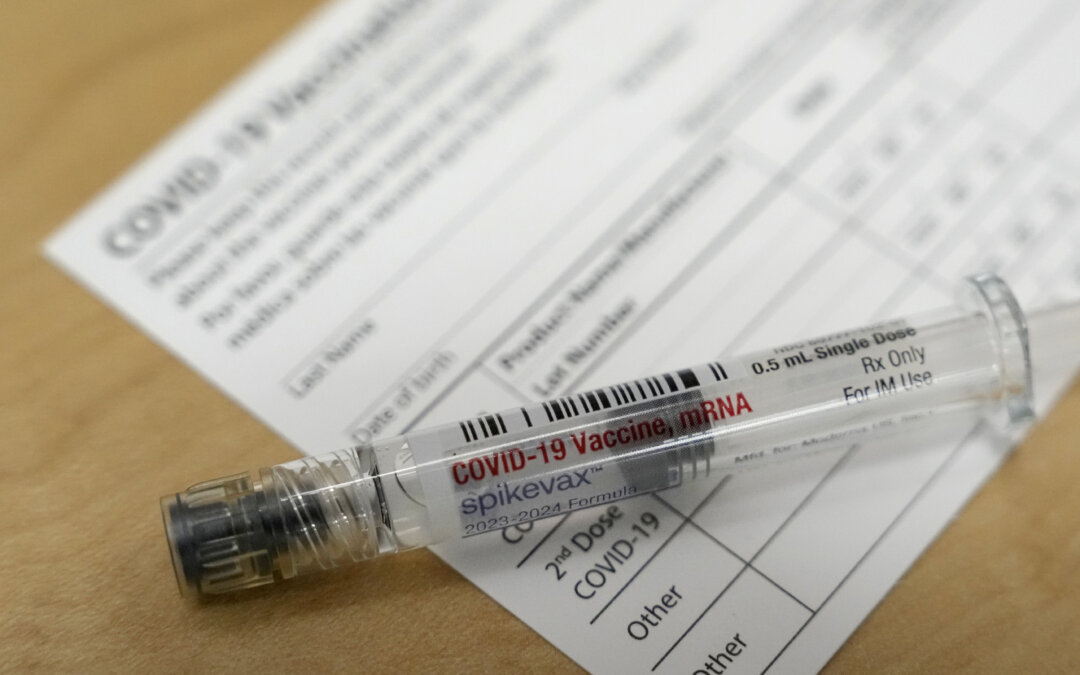
A version of this story appeared in the Granite Post's newsletter. Subscribe here. President Donald Trump announced Monday, Sept. 22 that the Food...

Fighting a health insurance denial? Here are 7 tips to help
By: Lauren Sausser When Sally Nix found out that her health insurance company wouldn’t pay for an expensive, doctor-recommended treatment to ease...
Health officials from 10 Northeast states officially band together. New Hampshire remains out.
By William Skipworth/ New Hampshire Bulletin This story was updated Sept. 19 to add a statement from a U.S. Department of Health and Human Services...

Portsmouth Regional Hospital opens cardiology clinic in Dover
Portsmouth Regional Hospital, part of HCA Healthcare, has opened a second location for cardiology services, providing patients with expanded options...

This woman from Keene says everyone will need to travel for care if local hospital closes—and she would know
Potential rural hospital closures loom in New Hampshire, after congressional Republicans and President Trump passed the “One Big Beautiful Bill Act”...

Dartmouth report IDs challenges of rural health care
By William Skipworth/ NH Bulletin Dr. Joanne Conroy, president and CEO of Dartmouth Health, wrote in a report released Friday that a recent meeting...




